Abstract
Background
Readmission rates after pneumonia, heart failure, and acute myocardial infarction hospitalizations are risk-adjusted for age, gender, and medical comorbidities and used to penalize hospitals.
Objective
To assess the impact of disability and social determinants of health on condition-specific readmissions beyond current risk adjustment.
Design, Setting, and Participants
Retrospective cohort study of Medicare patients using 1) linked Health and Retirement Study-Medicare claims data (HRS-CMS) and 2) Healthcare Cost and Utilization Project State Inpatient Databases (Florida, Washington) linked with ZIP Code-level measures from the Census American Community Survey (ACS-HCUP). Multilevel logistic regression models assessed the impact of disability and selected social determinants of health on readmission beyond current risk adjustment.
Main Measures
Outcomes measured were readmissions ≤30 days after hospitalizations for pneumonia, heart failure, or acute myocardial infarction. HRS-CMS models included disability measures (activities of daily living [ADL] limitations, cognitive impairment, nursing home residence, home healthcare use) and social determinants of health (spouse, children, wealth, Medicaid, race). ACS-HCUP model measures were ZIP Code-percentage of residents ≥65 years of age with ADL difficulty, spouse, income, Medicaid, and patient-level and hospital-level race.
Key Results
For pneumonia, ≥3 ADL difficulties (OR 1.61, CI 1.079–2.391) and prior home healthcare needs (OR 1.68, CI 1.204–2.355) increased readmission in HRS-CMS models (N = 1631); ADL difficulties (OR 1.20, CI 1.063–1.352) and ‘other’ race (OR 1.14, CI 1.001–1.301) increased readmission in ACS-HCUP models (N = 27,297). For heart failure, children (OR 0.66, CI 0.437–0.984) and wealth (OR 0.53, CI 0.349–0.787) lowered readmission in HRS-CMS models (N = 2068), while black (OR 1.17, CI 1.056–1.292) and ‘other’ race (OR 1.14, CI 1.036-1.260) increased readmission in ACS-HCUP models (N = 37,612). For acute myocardial infarction, nursing home status (OR 4.04, CI 1.212–13.440) increased readmission in HRS-CMS models (N = 833); ‘other’ patient-level race (OR 1.18, CI 1.012–1.385) and hospital-level race (OR 1.06, CI 1.001–1.125) increased readmission in ACS-HCUP models (N = 17,496).
Conclusions
Disability and social determinants of health influence readmission risk when added to the current Medicare risk adjustment models, but the effect varies by condition.
Similar content being viewed by others
The Centers for Medicare and Medicaid Services (CMS) seek to reduce readmissions by holding hospitals financially accountable using condition-specific risk-adjusted rates.1 , 2 Current CMS risk-adjustment models for readmission include patient characteristics from routine administrative data (e.g., age, gender, diagnosis codes).1 , 3 – 6 Disability and social determinants of health are not currently included in CMS risk adjustment, because they are not available in administrative data and there is concern that their inclusion may condone providing worse care to vulnerable populations.7 However, an increasing body of literature reveals that patient disability and social determinants of health impact readmission risk and vary across hospital populations, contributing to higher readmission penalties for safety-net hospitals—and generating increasing interest in studying risk adjustment for sociodemographic factors.1 , 8 – 26
To provide a better understanding of the extent to which the addition of patient disability and social determinants of health would impact the current risk adjustment models used by CMS, the objective of our study was to assess how measures of disability and social determinants of health were associated with readmission risk when used to enhance the current CMS condition-specific readmission models for pneumonia, heart failure, and acute myocardial infarction. We hypothesized that disability would predict readmission for both acute and chronic conditions. We also hypothesized that social determinants of health such as social support and wealth would be more important predictors of readmissions for chronic illnesses requiring complex home care, such as heart failure, than for acute illnesses like pneumonia.
METHODS
Conceptual Model
Figure 1 presents our conceptual model of predictors of readmission, including factors modifiable by the hospital (hospital course, discharge conditions and medications, and arrangement of post-discharge services) and patient factors less modifiable by the hospital, including those in the current CMS model (age, gender, and comorbidities) and the measures of disability and social determinants of health studied in this analysis. These patient factors influence readmission risk because they affect the patient’s ability to comply with the post-discharge treatment plan.
Conceptual model for disability and social determinants of health as predictors of readmission. Data sources for the predictor variables of interest in this study are indicated in parentheses. PT, physical therapy; SNF, skilled nursing facility; CMS, Centers for Medicare and Medicaid Services; HRS, Health and Retirement Study; ACS, American Community Survey; HCUP, Healthcare Cost Utilization Project.
Data Sources and Measures of Disability and Social Determinants of Health
To address our objective, we used two datasets that merge administrative data and survey data containing disability and social determinants of health measures.
Health and Retirement Study (HRS)27 Data Linked with Medicare Data: HRS-CMS
The HRS is an ongoing biennial cohort study of US residents over the age of 50, including measures of physical health and detailed interview surveys of factors impacting health, happiness, and finances, with over 35,000 participants interviewed. Participants are re-interviewed every 2 years, with >90 % follow-up rates and an 80.5 % overall cohort retention rate.28 We studied hospitalizations between June 1996 and June 2012 linked with Medicare Inpatient Standard Analytic Files and at least one pre-admission interview in 1995–2010 HRS data. Each index hospitalization was linked to that patient’s measures of disability and social determinants of health collected in the most recent survey before hospitalization.
Disability measures from HRS employed in this study included activities of daily living (ADL) limitations and cognitive function. At each survey, HRS asks respondents or proxies to report health-related difficulties with ADLs. Composite scores for ADL difficulty were computed and cut-offs determined a priori to represent no limitations (0), mild/moderate limitations (1–2), and severe limitations (3 or more). The HRS tests cognitive function using well-described methods;29 – 33 final models used a binary measure to describe patients as having no cognitive impairment versus any cognitive impairment. Two binary measures related to disability were obtained from the HRS data: whether the patient required nursing home services during the most recent HRS interview, or had used home health care services in the 2 years prior to the interview.
Social determinants of health from HRS included binary indicators for presence of spouse/partner, presence of children, and Medicaid receipt, and categorical indicators for wealth and race. Total household wealth was calculated as the sum of wealth components minus debt, in nominal dollars,34 converted to 2012 dollars for all waves;35 wealth quartiles were computed and assigned to account for non-linear effects and meaningful negative and zero values. Medicaid insurance, in addition to Medicare, was studied as an indicator of limited wealth, but it could also be an indicator of disability severity. Self-reported race was coded as white, black/African-American, or other. Age and gender were included in the current CMS risk adjustment, so they were not examined as individual predictors.
Census Data (American Community Survey, ACS) Merged with Healthcare Cost and Utilization Project Data: ACS-HCUP
Because the types of patient-specific measures in the HRS to enhance CMS data are not currently available nationwide, we tested whether publicly available community-level measures of disability and social determinants of health from Census data would be significant predictors of readmission when used to enhance CMS models for pneumonia, heart failure, and acute myocardial infarction. Five-year estimates of ZIP Code-level measures of resident disability and social characteristics were obtained from the American Community Survey (ACS) to merge with patient-level and hospitalization-level data from the Healthcare Cost and Utilization Project (HCUP). ACS is the largest nationally representative survey to provide annual updates to the decennial Census, with 97.3–98.0 % response rates for years studied.36 HCUP State Inpatient Databases (SIDs) are statewide databases containing administrative data generated by hospitals to request payment per calendar year. HCUP SIDs for Florida and Washington (2009–2012) were used, due to the ability to track patients and identify patient ZIP Code. Patient ZIP was used to link the HCUP claims record to the ACS 2008–2012 5-year estimates for the ZIP Code Tabulation Area (ZCTA)-level data for respondents aged 65 and older, the greatest geographical precision allowable for use with HCUP data.
The ACS measure of ADL disability was the percentage of respondents aged 65 and older indicating they had “difficulty dressing or bathing.” ACS cognitive difficulty measures were highly collinear with the ADL measure, so they were not included in the models. Candidate ACS measures for social determinants of health included several household composition and socioeconomic status variables that were highly collinear; we included the ZCTA-level measures of percentage of respondents aged 65 and older indicating they were married, in the highest income quartile, and with Medicaid. Patient-specific and hospital-level measures of race from HCUP were included.
Identification of Index Admission, Readmissions, and Medical Comorbidities
HRS-CMS linked Medicare claims data for 1996–2012 were processed using the readmissions measures code made publicly available by CMS,37 applying the same criteria as CMS for identifying index admissions for pneumonia, heart failure, and acute myocardial infarction unplanned readmissions within 30 days and exclusion criteria.6 Following CMS policy, exclusions included persons less than 65 years of age, lacking continuous enrollment in fee-for-service Medicare for 12 months pre-admission and 30 days post-admission, discharges against medical advice, and death within 30 days post-admission. Comorbidities included in current CMS models were abstracted from Medicare inpatient and outpatient claims data for the year prior to index admission. Patient age, gender, and race from index admission data were included. The same exclusions were applied to the ACS-HCUP cohorts, except for two not available in HCUP: continuous enrollment criteria and death <30 days of discharge. Readmissions were studied for admissions in 2012 with clinical comorbidities from 3 years’ prior HCUP discharge diagnoses (2009–2011) to mirror the current CMS model specifications due to no linkable outpatient data in HCUP.
Model Development and Statistical Analyses
To replicate current Medicare adjustments, coefficients for comorbidities, age, and gender were taken from current CMS readmission models for pneumonia, heart failure, and acute myocardial infarction.6 As these coefficients were derived from national Medicare claims data, and are presently used to determine extant hospital-level penalties, we did not recalibrate these coefficients with our HRS or HCUP cohorts. Our empty model included only an offset for individual readmission risk according to the current CMS condition-specific models. We first estimated the impact of disability and social determinants of health from HRS in individual predictor models that included only one HRS variable and the offset for CMS readmission risk including age, gender, and comorbidities. Full models were fit including all individual predictor variables from HRS and the offset for CMS readmission risk. An effect for time was also included to capture secular trends in condition-specific treatment and hospitalization. We used a similar modeling process to estimate individual predictor and full models using ACS-HCUP data.
For all models, multilevel mixed effects logit models were used; in HRS-CMS models, we accounted for within-patient variation, and in ACS-HCUP models for within-hospital variation. All analyses were conducted using xtmelogit in Stata 13.1.38 As HRS-CMS models covered the period 1996–2012, secular temporal trends were controlled with a linear time variable in all models. Two-tailed significance testing with a p value <0.05 was considered statistically significant. Odds ratios are reported with 95 % confidence intervals. We assessed model fit and performance in two ways: first, we compared the c-statistics of our full models to those published by CMS for current CMS risk adjustment; and second, we compared our models containing only the offset for clinical risk adjustment (as with the CMS models) to our full models containing disability and social determinants of health variables using likelihood ratio tests.
Human Subjects
The University of Michigan Institutional Review Board approved this study. HRS respondents provided informed consent for HRS participation and separate consent for linking their responses with CMS claims data. HCUP data are de-identified and publicly available. All HCUP Data Use Agreement conditions were followed.
RESULTS
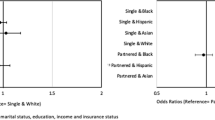
The application of inclusion/exclusion criteria to generate the analytic data sets is detailed in study flow diagrams in the Online Appendix Figures 1–6. Summary statistics for the disability measures and social determinants of health for the HRS-CMS and ACS-HCUP-derived cohorts are in Online Appendix Tables 1 and 2. Some social determinants varied by index condition; 66 % of heart failure cohort patients in HRS-CMS were in the lowest two wealth quartiles. Online Appendix Tables 3 and 4 summarize these cohorts’ clinical comorbidities from administrative data. Figures 2 and 3 and Online Appendix Figure 7 are coefficient plots illustrating the individual predictor and full-model results side by side for pneumonia, heart failure, and acute myocardial infarction. Panel A of each figure shows HRS-CMS data results; Panel B shows ACS-HCUP data results. Full-model results are provided in Table 1 (HRS-CMS) and Table 2 (ACS-HCUP). Cohort-specific average marginal effects, which provide information on the average change in predicted probability of readmission for changes in predictor variables of interest, are presented in Online Appendix Table 5.
Coefficient plots for pneumonia for both HRS-CMS and ACS-HCUP. HRS-CMS refers to Health and Retirement Study data linked with administrative claims data from the Centers for Medicare and Medicaid Services. ACS-HCUP refers to merged Healthcare Cost Utilization Project State Inpatient Databases from Florida and Washington (2009–2012) and US Census American Community Survey 5-year ZIP Code Tabulation Area (ZCTA) data, 2008–2012. Individual predictor models reflect the addition of a single disability measure or social determinant of health to the current CMS risk adjustment, while the full models reflect the addition of all measures of interest in addition to the CMS risk adjustment. * p < 0.05.
Coefficient plots for heart failure for both HRS-CMS and ACS-HCUP. HRS-CMS refers to Health and Retirement Study data linked with administrative claims data from the Centers for Medicare and Medicaid Services. ACS-HCUP refers to merged Healthcare Cost Utilization Project State Inpatient Databases from Florida and Washington (2009–2012) and US Census American Community Survey 5-year ZIP Code Tabulation Area (ZCTA) data, 2008–2012. Individual predictor models reflect the addition of a single disability measure or social determinant of health to the current CMS risk adjustment, while the full models reflect the addition of all measures of interest in addition to the CMS risk adjustment. * p < 0.05.
Pneumonia Cohorts
In HRS-CMS data (1631 index pneumonia admissions, 252 readmissions; Table 1), the only statistically significant predictors of readmission in the full model were two measures of disability (Fig. 2, Panel A): having 3+ ADL difficulties and prior home health care utilization, with ORs of 1.61 (CI 1.079–2.391) and 1.68 (CI 1.204–2.355), respectively.
In ACS-HCUP data (27,297 index pneumonia admissions, 3640 readmissions; Table 2), the only statistically significant predictors of readmission in the full model were ADL difficulties, with a 10-percentage-point increase in ADL difficulties among those 65 and older associated with a 1.20 increase in odds of readmission (CI 1.063-1.352) in the full model, all else equal (Table 2), and ‘other’ patient race (OR 1.14, CI 1.001–1.301). Other variables (marital status, higher income, Medicaid use, and patient race) were significantly associated with readmission when tested as individual predictors, but not in full models (Fig. 2, Panel B).
Heart Failure Cohorts
In HRS-CMS data (2068 index heart failure admissions, 487 readmissions; Table 1), only having children (OR 0.66, CI 0.437-0.984) and being in the highest quartile of wealth (OR 0.53, CI 0.349-0.787) remained statistically significant predictors of reduced readmission in the full model, despite many other variables appearing significant in individual predictor models (Fig. 3, Panel A).
In ACS-HCUP data (37,612 index heart failure admissions, 6697 readmissions; Table 2), only non-white patient race remained a statistically significant readmission predictor (black: OR 1.17, CI 1.056-1.292; other: OR 1.14, CI 1.036-1.260) in the full model, despite many variables appearing significant when tested in individual predictor models (Fig. 3, Panel B).
Acute Myocardial Infarction Cohorts
In HRS-CMS data (833 index admissions for acute myocardial infarction, 136 readmissions; Table 1), readmission rates declined significantly over the study period (OR 0.94; CI 0.893–0.990) in the full model. Only the infrequent status (N = 18) of nursing home residence during their most recent HRS interview was a statistically significant predictor of readmission (OR 4.04; CI 1.212–13.440) in the full model (Online Appendix Figure 7, Panel A).
In ACS-HCUP data (17,496 index admissions for acute myocardial infarction, 2452 readmissions; Table 2), only race remained a significant predictor of readmission in the full model (Table 2), both as patient-level race when identified in ACS data as ‘other’ (OR 1.18, CI 1.012–1.385) and the percentage of hospital patients listed as black or African-American in HCUP administrative data (OR 1.06, CI 1.001–1.125), despite many variables appearing significant when tested in individual predictor models (Online Appendix Figure 7, Panel B).
Model Fit and Performance
C-statistics for full HRS-CMS models were higher than those reported by CMS, but lower for ACS-HCUP models, by 0.01–0.06 (Table 3). For all ACS-HCUP cohorts and HRS-CMS pneumonia and heart failure cohorts, likelihood ratio tests indicated that the full model significantly improved model fit for our data relative to the model including only the clinical risk adjustment.
DISCUSSION
Our study is the first to assess measures of disability and social determinants of health as enhancements to the CMS condition-specific models currently used for comparing and penalizing hospitals, as opposed to studies employing the all-cause hospital readmission model.19 , 23 By employing three condition-specific models as opposed to one all-cause readmission model, our results enable us to compare and contrast the effects of these patient characteristics on readmission risk by condition. The results illustrate that the additional predictive effects these disability and social determinants of health have on readmission risk varies by the condition for index admission. Many disability and social determinants of health variables appear significant when tested as individual predictors beyond administrative data-derived comorbidities, yet are no longer significant in full condition-specific models. No predictors were significant across all three conditions. We also studied the condition-specific models using two different data sets of merged administrative and survey data, to examine differences in the impact of patient-level and community-level measures of disability and social determinants of health on readmission risk.
We had hypothesized that disability limitations measured as ADL limitations would be significant predictors of readmission for all the cohorts, supported by literature data.10 – 19 , 39 – 42 Although ADL limitations were significant predictors of readmission for pneumonia using the HRS-CMS and ACS-HCUP data sets, this was not demonstrated for the heart failure or acute myocardial infarction cohorts. Cognitive impairment did not predict readmission in any cohort for either data set, perhaps because the diagnosis of dementia is part of the standard CMS risk adjustment already applied.
We hypothesized that social determinants of health may be important in predicting readmission for chronic conditions such as heart failure, requiring complex medications, diet, and follow-up. This was supported in the heart failure full models using patient-level HRS-CMS dataset, with significant associations noted for having children and being in the highest quartile of wealth. In the HRS-CMS sample for heart failure, 66 % of patients were in the lowest two quartiles of wealth. Returning to our conceptual model, we could imagine two hypothetical patients admitted for heart failure of identical age, gender, and medical comorbidities, but who differed with respect to disability and social profiles, moderating their ability to comply with post-discharge instructions. While the current CMS model would assign the same probability of readmission to both patients, our enhanced risk model for heart failure would predict a probability of readmission 23 percentage points higher for an African-American patient with significant ADL limitations that lives alone and has little wealth, compared to a white, married patient with no ADL limitations and high wealth, net differences in comorbidities (95 % CI 0.09–0.36).
Minority race was a significant predictor impacting hospital readmission rates for all cohorts in the ACS-HCUP dataset as supported by the literature.43 Yet, race was not predictive in the smaller HRS-CMS dataset, and there are concerns about the accuracy of the race variable in HCUP data, particularly as it is not required or audited in standard hospital claims data.44 , 45
Our study has several limitations. For HRS-CMS models, the use of condition-specific models yields fewer index admissions and readmissions per analytic cohort than prior analyses involving hospital-wide readmissions, which impacts our power to detect significant predictors. Due to the lag time (mean >460 days) between the most recent HRS survey and the index admission, more recent increases in baseline disability before admission could not be studied, and could reduce the power to detect significant associations between increased disability and readmission risk. Social support measures were limited, because having a spouse or child may not necessarily mean that they provide assistance. Missing data involved 15.5–18.8 % of eligible HRS cases missing one or more predictor variables of interest, most commonly Medicaid eligibility, ADLs, or receipt of home health care. The effects of these variables may be less generalizable than variables with less missing data. For the ACS-HCUP models, HCUP data allowed examination of hospital-level compositional and random effects, but data from two states may not be representative of national trends. Further study should examine ACS predictors with nationally representative data such as the Medicare claims database. The lack of outpatient data and information on continuous enrollment in HCUP prevented the exact replication of CMS risk adjustment for readmission. HCUP analyses were limited to ZCTA-level ACS data rather than more precise geographic data. Census tract geographic coding may uncover different associations.
Disability and social determinants of health measures are not currently routinely collected for all Medicare beneficiaries. The Medicare Current Beneficiary Survey46 obtains these measures for a sample of beneficiaries. However, hospitals routinely collect measures of disability and social determinants of health for admission assessments, discharge planning, and Medicare Annual Wellness Visits that could be used to enrich Medicare claims data.
Conclusion
The impact of disability and social determinants of health beyond the current risk adjustment provided in CMS condition-specific models is complex and varies by condition. Our results suggest that a first priority may be to focus on the inclusion of disability measures such as ADL limitations and nursing home needs (already extensively documented in electronic medical records) as additions to comorbidities for risk adjustment when considering the average marginal effect of these characteristics, data collection feasibility, and complexities involving accuracy and implications for adjustment of race, income, and social support variables.
References
Accounting for Social Risk Factors in Medicare Payment: Identifying Social Risk Factors. Washington, DC: National Academies of Sciences, Engineering, and Medicine. 2016. Available at http://www.nap.edu/catalog/21858/accounting-for-social-risk-factors-in-medicare-payment-identifying-social. Accessed September 9, 2016.
Boccuti C, Casillas G. Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. Menlo Park, CA: The Henry J. Kaiser Family Foundation; 2015. Available at http://slcsuperiorhomecare.com/wp-content/uploads/2015/06/Kaiser-Readmission-paper.pdf. Accessed September 9, 2016.
Krumholz H, Normand SL, Keenan P, et al. Hospital 30-day Heart Failure Readmission Measure: Methodology. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE); 2008. Available at http://www.qualitynet.org/. Accessed September 9, 2016.
Krumholz HM, Normand SL, Keenan PS, et al. Hospital 30-Day Pneumonia Readmission Measure: Methodology. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE); 2008. Available at http://www.qualitynet.org/. Accessed September 9, 2016.
Krumholz HM, Normand SL, Keenan PS, et al. Hospital 30-Day Acute Myocardial Infarction Readmission Measure: Methodology. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE); 2008. Available at http://www.qualitynet.org/. Accessed September 9, 2016.
Grady JN, Lin Z, Wang C, et al. Measures Updates and Specifications Report: Hospital-Level 30-Day Risk-Standardization Readmission Measures for Acute Myocardial Infarction, Heart Failure, and Pneumonia. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE); 2013. Available at http://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/Measure-Methodology.html. Accessed September 9, 2016.
Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation (YNHHSC/CORE). 2013 Measures Updates and Specifications Report: Hospital-Level 30-Day Risk-Standardized Readmission Measures for Acute Myocardial Infarction, Heart Failure, and Pneumonia (Version 6.0). 2013. Available at https://www.qualitynet.org/dcs/ContentServer?cid=1228774371008&pagename=QnetPublic%2FPage%2FQnetTier4&c=Page. Accessed September 9, 2016.
H.R. 4994 (113th): IMPACT Act of 2014. Pub.L. 113-185. Signed October 6, 2014. Available at https://www.govtrack.us/congress/bills/113/hr4994, accessed September 9, 2016.
Medicare Payment Advisory Commission. Refining the hospital readmissions reduction program. Washington, D.C: Medicare Payment Advisory Commission; 2013. Available at http://www.medpac.gov/docs/default-source/reports/jun13_ch04.pdf. Accessed September 9, 2016.
Calvillo–King L, Arnold D, Eubank KJ, et al. Impact of social factors on risk of readmission or mortality in pneumonia and heart failure: systematic review. J Gen Intern Med. 2013;28(2):269–82.
Chin MH, Goldman L. Correlates of early hospital readmission or death in patients with congestive heart failure. Am J Cardiol. 1997;79(12):1640–4.
Coleman EA, Min SJ, Chomiak A, Kramer AM. Post-hospital care transitions: patterns, complications, and risk identification. Health Serv Res. 2004;39(5):1449–65.
Kansagara D, Englander H, Salanitro A, et al. Risk prediction models for hospital readmission: a systematic review. JAMA. 2011;306(15):1688–98.
Smith DM, Katz BP, Huster GA, Fitzgerald JF, Martin DK, Freeman JA. Risk factors for non-elective hospital readmissions. J Gen Intern Med. 1996;11(12):762–4.
DePalma G, Xu H, Covinsky KE, et al. Hospital readmission among older adults who return home with unmet need for ADL disability. Gerontologist. 2012;53(3):454–61.
Fisher SR, Kuo YF, Sharma G, et al. Mobility after hospital discharge as a marker for 30-day readmission. J Gerontol A Biol Sci Med Sci. 2013;68(7):805–10.
Garcia-Perez L, Linertova R, Lorenzo-Riera A, Vazquez-Diaz JR, Duque-Gonzalez B, Sarria-Santamera A. Risk factors for hospital readmissions in elderly patients: a systematic review. QJM. 2011;104(8):639–51.
Shih SL, Gerrard P, Goldstein R, et al. Functional status outperforms comorbidities in predicting acute care readmissions in medically complex patients. J Gen Intern Med. 2015;30(11):1688–95.
Barnett ML, Hsu J, McWilliams JM. Patient characteristics and differences in hospital readmission rates. JAMA Intern Med. 2015;175(11):1803–12.
McCoy JL, Davis M, Hudson RE. Geographic patterns of disability in the United States. Soc Secur Bull. 1994;57(1):25–36.
Oddone EZ, Weinberger M, Horner M, et al. Classifying general medicine readmissions. Are they preventable? Veterans Affairs Cooperative Studies in Health Services Group on Primary Care and Hospital Readmissions. J Gen Intern Med. 1996;11(10):597–607.
Joynt KE, Jha AK. Thirty-day readmissions - truth and consequences. N Engl J Med. 2012;366(15):1366–9.
Greysen SR, Cenzer IS, Auerbach AD, Covinsky KE. Functional impairment and hospital readmission in Medicare seniors. JAMA Intern Med. 2015;175(4):559–65.
Berenson J, Shih A. Higher Readmissions at Safety-Net Hospitals and Potential Policy Solutions. New York, NY: The Commonwealth Fund; 2012. Available at http://www.commonwealthfund.org/publications/issue-briefs/2012/dec/higher-readmissions-and-potential-policy-solutions. Accessed September 9, 2016.
Risk Adjustment for Socioeconomic Status or Other Sociodemographic Factors Washington, DC: National Quality Forum. 2014. Available at http://www.qualityforum.org/Publications/2014/08/Risk_Adjustment_for_Socioeconomic_Status_or_Other_Sociodemographic_Factors.aspx. Accessed September 9, 2016.
To amend title XVIII of the Social Security Act to improve the risk adjustment under the Medicare Advantage program, and for other purposes., House of Representatives. 2015.
Health and Retirement Study: An Introduction. 2016. Available at http://hrsonline.isr.umich.edu/index.php?p=intro. Accessed September 9, 2016.
Health and Retirement Study. Sample Sizes and Response Rates. Ann Arbor, MI. 2011. Available at http://hrsonline.isr.umich.edu/sitedocs/sampleresponse.pdf. Accessed September 9, 2016.
Langa KM, Chernew ME, Kabeto MU, et al. National estimates of the quantity and cost of informal caregiving for the elderly with dementia. J Gen Intern Med. 2001;16(11):770–8.
Langa KM, Larson EB, Karlawish JH, et al. Trends in the prevalence and mortality of cognitive impairment in the United States: is there evidence of a compression of cognitive morbidity? Alzheimers Dement. 2008;4(2):134–44.
Langa KM, Plassman BL, Wallace RB, et al. The Aging, Demographics, and Memory Study: study design and methods. Neuroepidemiology. 2005;25(4):181–91.
Ofstedal MB, Fisher GG, Herzog AR. Documentation of cognitive functioning measures in the Health and Retirement Study. Ann Arbor, MI: University of Michigan; 2005.
Iwashyna TJ, Ely EW, Smith DM, Langa KM. Long-term cognitive impairment and functional disability among survivors of severe sepsis. JAMA. 2010;304(16):1787–94.
Chien S, Campbell N, Hayden O, et al. RAND HRS Data Documentation, Version N. Labor & Population Program, RAND Center for the Study of Aging. 2014.
Bureau of Labor Statistics. CPI Inflation Calculator. 2016. Available at http://www.bls.gov/data/inflation_calculator.htm. Accessed September 9, 2016.
U.S. Census Bureau. American Community Survey: Sample Size and Data Quality. 2015. Available at http://www.census.gov/acs/www/methodology/sample-size-and-data-quality/response-rates/. Accessed September 9, 2016.
ReadmissionAMI_HF_PN_SASPACK. 1 ed. Baltimore, MD: Centers for Medicare & Medicaid Services; 2013.
StataCorp. Stata Statistical Software: Release 13. College Station, TX: StataCorp LP; 2013.
Allman RM, Goode PS, Patrick MM, Burst N, Bartolucci AA. Pressure ulcer risk factors among hospitalized patients with activity limitation. JAMA. 1995;273(11):865–70.
Bergquist S, Frantz R. Pressure ulcers in community-based older adults receiving home health care. Prevalence, incidence, and associated risk factors. Adv Wound Care. 1999;12(7):339–51.
De Brauwer I, Lepage S, Yombi JC, Cornette P, Boland B. Prediction of risk of in-hospital geriatric complications in older patients with hip fracture. Aging Clin Exp Res. 2012;24(1):62–7.
Holicky R, Charlifue S. Ageing with spinal cord injury: The impact of spousal support. Disabil Rehabil. 1999;21(5/6):250–7.
Joynt KE, Orav EJ, Jha AK. Thirty-day readmission rates for Medicare beneficiaries by race and site of care. J Am Med Assoc. 2011;305(7):675–81.
Andrews R. The quality of reporting on race & ethnicity in US hospital discharge abstract data. Agency for Healthcare Research and Quality; June 10, 2008.
Defining Categorization Needs for Race and Ethnicity Data. Rockville, MD: Agency for Healthcare Research and Quality. October 2014. Available at http://www.ahrq.gov/research/findings/final-reports/iomracereport/reldata3.html. Accessed September 9, 2016.
Centers for Medicare & Medicaid Services. Medicare Current Beneficiary Survey. 2016. Available at https://www.cms.gov/Research-Statistics-Data-and-Systems/Research/MCBS/index.html?redirect=/mcbs. Accessed September 9, 2016.
Acknowledgments
Primary Funding Source
Agency for Healthcare Research and Quality
Author Contributions
Dr. Meddings, Ms. Reichert, and Dr. Smith had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Meddings, McMahon, Reichert, Smith
Acquisition of data: Meddings, Reichert, Smith, Langa, Iwashyna
Analysis and/or interpretation of data: Meddings, McMahon, Reichert, Smith, Langa, Iwashyna
Drafting of the manuscript: Meddings, McMahon, Reichert, Smith
Critical revision of the manuscript for important intellectual content: Meddings, McMahon, Reichert, Smith, Langa, Iwashyna, Hofer
Statistical analysis: Reichert, Smith
Obtaining funding: Meddings, McMahon
Study supervision: Meddings, McMahon
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funders
This work was funded by the Agency for Healthcare Research and Quality (AHRQ; 2R01HS018334, 1K08HS019767). The funding sources were not involved in the conduct, interpretation, or reporting of the results, or the decision to submit the manuscript for publication. The Health and Retirement Study is funded by the National Institute on Aging (U01 AG009740), and performed at the Institute for Social Research, University of Michigan.
Disclaimer
The findings and conclusions in this report are those of the authors and do not necessarily represent those of the sponsor, AHRQ, the US Government, or the Department of Veterans Affairs.
Contributors
We thank Jessica Ameling, MPH, and Laura Petersen, MHSA, for providing assistance with references and manuscript editing. We are very appreciative for the insights and expertise provided by Mary A.M. Rogers, PhD, for the development of the grant, use of HRS-CMS data, and analyses.
Prior Presentations
These analyses were presented in part as posters at the Society of General Internal Medicine Annual Meeting, Toronto, Ontario, on April 23, 2015; the AcademyHealth Annual Research Meeting, Minneapolis, Minnesota, on June 14, 2015; and the International Conference on Health Policy Statistics, Providence, Rhode Island, on October 8, 2015.
Conflict of Interest
All authors have completed and submitted the ICJME Form for Disclosure of Potential Conflicts of Interest. Dr. Meddings has reported receiving honoraria for lectures and teaching related to prevention and value-based purchasing policies involving catheter-associated urinary tract infection and hospital-acquired pressure ulcers. The remaining authors report no conflicts of interest.
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Appendix Table 1
Summary statistics for HRS-CMS patients for readmission, demographics, disability, and social determinants of health variables, by cohort, N (%) (DOCX 37 kb)
Appendix Table 2
Summary statistics for ACS-HCUP patients for readmission, demographics, disability, and social determinants of health variables, by cohort, N (%) (DOCX 41 kb)
Appendix Table 3
HRS-CMS prevalence of clinical comorbidities by cohort, N (%) (DOCX 40 kb)
Appendix Table 4
ACS-HCUP prevalence of clinical comorbidities by cohort, N (%) (DOCX 41 kb)
Appendix Table 5
Average marginal effects for HRS-CMS models, by cohort (DOCX 38 kb)
Appendix Figure 1
Study flow diagram for HRS-CMS pneumonia cohort (DOCX 294 kb)
Appendix Figure 2
Study flow diagram for HRS-CMS heart failure cohort (DOCX 294 kb)
Appendix Figure 3
Study flow diagram for HRS-CMS acute myocardial infarction cohort (DOCX 301 kb)
Appendix Figure 4
Study flow diagram for ACS-HCUP pneumonia cohort (DOCX 130 kb)
Appendix Figure 5
Study flow diagram for ACS-HCUP heart failure cohort (DOCX 131 kb)
Appendix Figure 6
Study flow diagram for ACS-HCUP acute myocardial infarction cohort (DOCX 133 kb)
Appendix Figure 7
Coefficient plots for acute myocardial infarction for both HRS-CMS and ACS-HCUP (DOCX 13.0 mb)
Rights and permissions
About this article
Cite this article
Meddings, J., Reichert, H., Smith, S.N. et al. The Impact of Disability and Social Determinants of Health on Condition-Specific Readmissions beyond Medicare Risk Adjustments: A Cohort Study. J GEN INTERN MED 32, 71–80 (2017). https://doi.org/10.1007/s11606-016-3869-x
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11606-016-3869-x